The comorbidity between Feeding and Eating Disorders and Personality Disorders: A systematic review of current status
Giulia Spinielloa, Walter Sapuppoa,b
a Department of Psychology, Sigmund Freud University, Milan, Italy
b School of Applied Sciences, London South Bank University, London, U.K
Riassunto
Obiettivo: aggiornare lo stato dell’arte circa la comorbilità tra Disturbi della Nutrizione e dell’Alimentazione (DNA) e Disturbi di Personalità (DP), facendo riferimento al modello categoriale delle ultime versioni del Manuale Statistico e Diagnostico dei Disturbi Mentali (DSM): DSM-IV, DSM-IV-TR and DSM-5. La seguente revisione sistematica della letteratura è stata condotta a partire dall’anno 2014, al quale è possibile far risalire gli ultimi articoli sull’argomento.
Metodo: la seguente revisione sistematica è stata condotta secondo le linee guida PRISMA. Sono state eseguite ricerche sistematiche avanzate su PubMed e EBSCOhost, utilizzando la seguente stringa di ricerca: (eating disorders or anorexia or bulimia or binge eating) AND personality disorder AND (comorbidity or comorbidities or cooccurrence or comorbid) NOT (review of literature or literature review or meta-analysis or systematic review). La seguente strategia di ricerca ha permesso di raccogliere 4 studi da includere nella seguente revisione, nell’intervallo tra Febbraio 2014 e Marzo 2022.
Risultati: l’analisi dei 4 studi suggerisce una comorbilità tra i DNA e i DP. Mentre questa co-occorrenza sembra prevalere in una popolazione normale, la pre-esistenza di disturbi psichiatrici come ADHD o ASD non sembra avere impatto nella comorbilità tra le due patologie.
Discussione: studi più approfonditi riguardo la co-occorrenza generale tra DNA e DP potrebbero essere d’aiuto per aggiornare e sintetizzare i risultati su questo tema complicato, non solo per aggiornare lo stato dell’arte, ma anche per essere pronti a trattare queste patologie in costante evoluzione.
Parole chiave
Disturbi della Nutrizione e dell’Alimentazione
Disturbi di Personalità
Comorbilità
Approccio categoriale
Revisione sistematica
Abstract
Purpose of review: to update the state of art about the comorbidity between Feeding and Eating Disorders (FEDs) and Personality Disorders (PDs), referring to the categorical of the latest versions of the Statistical and Diagnostic Manual of Mental Disorders (DSM): DSM-IV, DSM-IV-TR and DSM-5. The following state-of-art literature review has been carried out since 2014, to which is possible to trace the latest findings about the topic.
Methods: the present systematic review has been conducted in accordance to PRISMA guidelines. Advanced systematic searches in PubMed and EBSCOhost have been conducted using the following search string with Boolean operators (eating disorders or anorexia or bulimia or binge eating) AND personality disorder AND (comorbidity or comorbidities or cooccurrence or comorbid) NOT (review of literature or literature review or meta-analysis or systematic review). The search strategy garnered four studies for inclusion in the present review, referred between February 2014 and March 2022.
Results: the analysis of the 4 studies suggests a comorbidity between FEDs and PDs. While this co-occurrence seems to prevail in a plain population, pre-existence of psychiatric disorders such as ADHD or ASD seem not to have an impact on the comorbidity between the two disorders.
Discussion: more in-depth studies on the general co-occurrence between FEDs and PDs can be really helpful to update and synthesise the results on this sketchy topic, not only for the purpose to bring up to date the literature, but also to be ready to treat such disorders that are constantly evolving.
Keywords
Eating disorders
Personality disorders
Comorbidity
Categorical approach
Systematic review
Introduction
The section on “Feeding and Eating Disorders” (FED; American Psychiatric Association – APA, 2013, p. 329) in the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5; APA, 2013), includes three specific diagnoses: “Anorexia Nervosa” (AN; APA, 2013), “Bulimia Nervosa” (BN; APA, 2013) and “Binge-Eating Disorder” (BED; APA, 2013) (Udo & Grilo, 2019). These are the three main FEDs (Udo & Grilo, 2019), the first topic studied in this review. FEDs, according to the diagnostic criteria of DSM-5 (APA, 2013), are characterized by a long-lasting eating disorder or eating behaviors, which result in irregular consumption or absorption of food and impaired physical health and psychosocial functioning (APA, 2013). Until now, FEDs have been studied mostly through “top-down” methodological mechanisms and therefore adapted to a priori study paradigms, inspired by empirical principles of simplification and reproducibility. However, this modus operandi, which will also be used in this review, risks not taking into account some masked factors given by the complex perniciousness and multifactoriality of the eating pathology, being in fact neither simple nor always equally expressed (Bertelli et al., 2019). In fact, FEDs are frequently double diagnoses from a psychopathological point of view: they are often associated with mood disorders, anxiety states, personality disorders, post-traumatic syndromes and other cognitive and metacognitive characteristics whose comorbidity further aggravates their complexity (Bertelli et al., 2019; Mitchell, Wolf, Reardon, & Miller, 2014; Sapuppo et al., 2018). Among these, the comorbidity between FEDs and “Personality Disorders” (PD; APA, 2013, p. 645) is perhaps the one most thoroughly researched and summarized in many meta-analysis (Rosenvinge, Martinussen, & Ostensen, 2000; Friborg et al., 2014; Martinussen et al., 2016) covering literature from 1983 to 2014 (Rosenvinge & Pettersen, 2015).
The second topic studied in this review are Personality Disorders. DSM-5 conceptualizes Personality Disorder as an “enduring pattern of inner experience and behaviour” that clearly diverges from the perspectives of the subject’s reference culture (APA, 2013, p. 645), is “inflexible and pervasive”, begins in adolescence or early adulthood, it is long-lasting and causes “distress or impairment” (APA, 2013, p. 646).
The PDs, according to the categorical classification included in Section II of the DSM-5, are grouped into three groups or ‘clusters’ based on similarities. Cluster A includes paranoid, schizoid, and schizotypal personality disorders. People with these disorders often appear strange or eccentric. Cluster B includes antisocial, borderline, histrionic, and narcissistic personality disorders. Individuals with these disorders often appear dramatic, emotional, or unpredictable. Cluster C includes avoidant, dependent and obsessive-compulsive personality disorders. Individuals with these disorders often appear anxious or fearful (APA, 2013). To diagnose a PD, it must occur with high frequency and involve a wide range of behaviours, feelings and perceptions in different contexts.
The literature was assessed in accordance with the PICOS process (Moher et al., 2015) as follows: P-Population: (i) Italian outpatients with a FED; (ii) sample of American adults; (iii) sample of Australian women; (iv) adults and young adults with pre-existing psychiatric problems. I-Intervention: not applied to any type of study. C-Comparison: (i) absence of a control group; (ii) group without FED; (iii) group without PD; (iv) group without FED. O-Outcome: (i) differences in the prevalence of comorbidities on the basis of gender; (ii) comorbidity of AN e BN to the BPD; BED to the STPD, BPD e APD; (iii) marked portion of comorbidity with FED in subjects with PD; (iv) absence of a significant difference in PD between subjects with and without FED. S-Study Design: (i) descriptive cross-sectional study; (ii) analytical cross-sectional study; (iii) analytical cross-sectional study; (iv) analytical cross-sectional study.
Methods and materials
The following review was conducted following the PRISMA guidelines (Preferred Reporting Items for Systematic Reviews and Meta-Analyses; Page et al., 2020)
Inclusion and Exclusion Criteria
Studies were included if they met the following criteria: (i) they were written in English; (ii) they started from 2014 (included); (iii) they reported information about the comorbidity between FEDs and the categorical classification of PDs; (iv) was reported a categorical classification of PDs. The following criteria were grounds for exclusion: (i) subjects under 18 years old; (ii) articles that were not written in English; (iii) the interviews used for the assessment were not standardized; (iv) the articles referred to “disordered eating” and not to “eating disorders”; (v) articles that did not meet the PRISMA inclusion criteria – marked as “Others”; (vi) articles marked as “Erratum”; (vii) articles that reported only a dimensional classification of PDs.
Information Source and Source Strategy
The literature search was conducted starting from 2014, year of publication of the last review on the argument (Martinussen et al., 2016), until March 2022 using the advanced search of the following open access databases: PubMed and EBSCOhost. The search string used is the following: (eating disorders or anorexia or bulimia or binge eating) AND personality disorder AND (comorbidity or comorbidities or cooccurrence or comorbid) NOT (review of literature or literature review or meta-analysis or systematic review). It is important to note the temporal inconsistency reported by the authors of the meta-analysis (2016) compared to that reported by the following systematic review of the literature (2014). After a careful analysis of the bibliography of the article by Martinussen and colleagues (2016) it emerged that, unlike what they reported, an analysis of the literature was carried out up to February 2014, a decision that led to starting the following systematic review from this date, trying to collect precisely the information present in the literature about the comorbidity between FEDs and PDs up to 2022.
Data Collection Process and Study Selection
The electronic literature searches and the selection of studies based on the methodology and appropriateness for inclusion followed the PRISMA guidelines (Page et al., 2020) and were subsequently reviewed by the other author. The research on both databases, PubMed and EBSCOhost, has produced numerous articles which have subsequently been reduced by inserting the time limitation “starting from 2014”. It was thus possible to analyse the articles resulting from the insertion of the filter, being temporally relevant to the purpose of the research. The next step included the elimination of duplicates. Once deleted, the articles were analysed, selecting them by title and abstract based on the degree of relevance to the research question. Each article that seemed to help answer the research question was therefore included in this passage. The latter were subjected to a further strict screening based on the eligibility criteria – inclusion and exclusion – indicated above. Finally, by subtracting the articles excluded for non-compliance with the criteria from the total number of articles reviewed for eligibility, the result was of four total articles. No restrictions were placed on the mental status of the subjects participating in the studies.
Results
The initial search, already filtered on a temporal basis, retrieved a total of 623 articles: 396 on EBSCOhost, 227 on PubMed. After removing the duplicates (n=210), were analysed the title and abstract of each article. 155 articles were excluded starting from the title, while 195 articles were excluded based on the abstract because: 93 of them concerned only FEDs, excluding comorbidity with PDs; 34 concerned only PDs excluding comorbidity with FEDs; 68 analysed a comorbidity that was beyond the scope of the research. 63 items remain, which have been skimmed in light of the eligibility criteria. At this stage of the process, 59 articles were excluded because: they were reviews or meta-analyses or books or dissertations (n=1); they used a dimensional classification of the PDs (n=14); non-standardized interviews were used (n=2); they were not in English (n=25); did not respect the lower limit of pre-established age (n=9); analysed a non-clinical category of FEDs (n=6); did not meet the PRISMA inclusion criteria and therefore marked with “Others” (n=1); they were articles marked as “Erratum” (n=1). Thus, in total, 4 articles were retained for the main body of the review (Figure 1). The details of the selected studies are presented in Tables I and II, which report the authors, the year of publication, the study design, the characteristics of the sample and the main results of each study.
The systematic review included four articles: three analytical cross-sectional studies (Udo & Grilo, 2019; Quirk et al., 2017; Karjalainen, Gillberg, Wentz, & Råstam, 2016) and a descriptive cross-sectional study (Valente et al., 2017). All four studies taken into consideration dealt with the co-occurrence between the two disorders in a not explicit way: some articles (Quirk et al., 2017; Valente et al., 2017) in fact, presented the possible co-occurrence found as a duty to further studies and insights. Other studies (Quirk et al., 2017; Udo & Grilo, 2019; Karjalainen, Gillberg, Wentz, & Råstam, 2016) instead, posed the following research question as a secondary objective: this led to a limited number of statistical analyses conducted and to a limited number of subjects taken into consideration.
Data Synthesis
Studies considerated adequate for inclusion criteria underwent a narrative review. Narrative reviews are a discussion of theoretically important topics (Jahan, Naveed, Zeshan, & Tahir, 2016) and aim to summarize the current state of the art considering a wide variety of sources (Popay et al., 2006).
Figure 1. Flow chart summarizing the study selection procedure
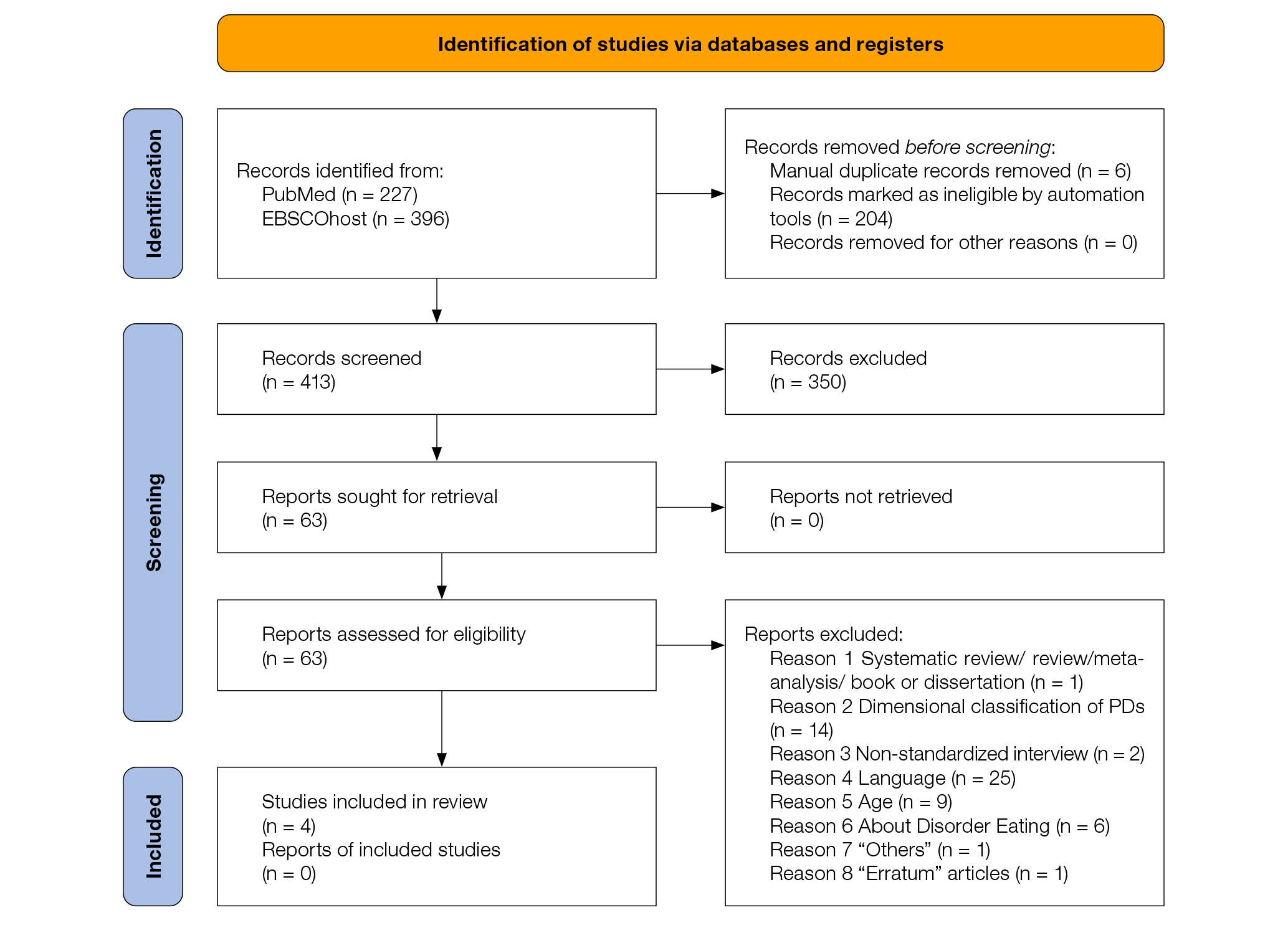
From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: 10.1136/bmj.n71
For more information, visit: http://www.prisma-statement.org/
Table I. Characteristics of the studies included in the systematic review
| Author and year | N | Diagnoses | Age | Country | N-% M and F | Reference population | Study design |
|---|---|---|---|---|---|---|---|
| (Valente et al., 2017) | 267 |
|
18-74 (M=37.3; SD ± 12,5) |
Italy |
|
Italian outpatients with ED | Descriptive cross-sectional study |
| (Udo & Grilo, 2019) | 36,309 |
|
>18 (M=45,6; SD = 17±5) |
USA |
|
Nationally representative sample of adults in the USA (non-Hispanic white; non-Hispanic black; Hispanic and “other” group | Analytical cross-sectional study |
| (Quirk et al., 2017) | 768 |
|
≥ 25 years (25-34) (35-44) (45-54) (55-64) (65-74) ≥ 75 |
Australia |
|
Age stratified sample of Australian women | Analytical cross-sectional study |
| (Karjalainen et al., 2016) |
228 (n=18; ED) (n=210; no ED) |
|
19-60 (M=31,75) |
Sweden |
|
Young adults and adults with ESSENCE and ED | Analytical cross-sectional study |
M=males; F=females; N=numerosity; AN=Anorexia Nervosa; BN=Bulimia Nervosa; BED=Binge-Eating Disorder; ED=Eating Disorder (ex DSM-IV-TR); PD=Personality Disorder; M=Mean; SD=Standard Deviation; ESSENCE=Early Symptomatic Syndromes Eliciting Neurodevelopmental Clinical Examinations (ex: ADHD, ASD, tic disorder)
§ = missing data regarding the number of people belonging to the specific diagnosis
Table II. Risults of individual studies
| Author and year | Diagnostic tools | Comparison | Comorbidity FED-PD | Main findings |
|---|---|---|---|---|
| (Valente et al., 2017) |
|
– |
BPD (F); OCPD ↔ AN PPD ↔ BED (M) |
PD cluster B: differences in prevalence based on gender: BPD → women with AN (p=0.001). PD cluster C: OCPD → AN (p<0.05). PD cluster A: PPD → BED (p=0.034) |
| (Udo & Grilo, 2019) |
|
Group without FED |
BPD ↔ AN, BN STPD, BPD, APD ↔ BED |
PD cluster B: (1) BPD (2) APD → (1) AN; BN (p<.01; p<.05) → (1) (2) BED (p<.01; p<.01) PD cluster A: STPD → BED (p<.01) |
| (Quirk et al., 2017) |
|
Group without PD |
PD ↔ ED (11.5%) PD → ED (2.8%) |
Subjects with PD (n=157) → marked portion of comorbidity with ED (n=18>; 11.5%) in the course of life compared to → subjects without PD (11% vs 2.8%). |
| (Karjalainen et al., 2016) |
|
Group without ED |
PD + ED = 12 (66.7%) PD + no ED = 104 (49,5%) |
There is no significant difference in PD between subjects with and without ED (p=0.22). |
FED=Feeding and Eating Disorder; ED=Eating Disorder (ex DSM-IV-TR); AN=Anorexia Nervosa; BN=Bulimia Nervosa; BED=Binge-Eating Disorder; PD=Personality Disorder; BPD=Borderline Personality Disorder; OCPD=Obsessive-Compulsive Personality Disorder; PPD=Paranoid Personality Disorder; STPD=Schizotypal Personality Disorder; APD=Antisocial Personality Disorder; SCID=Structured Clinical Interview for DSM; SCID-I=Structured Clinical Interview for DSM IV Axis I Disorders; SCID-I-NP=Structured Clinical Interview for DSM – Nonpatient version; SCID-II=Structured Clinical Interview for DSM IV Axis II; AUDADIS-5=Alcohol Use Disorder and Associated Disabilities Interview Schedule-5.
↔ = significantly associated; → = not associated; + = put in relation (with)
Discussion
Summary of Findings
The following systematic review was conducted with the aim of providing an updated, although not exhaustive, overview of the comorbidity between FED (AN, BN and BED) and the categorical diagnosis of PD.
This work produced five main findings. The first result is that the presence of a comorbidity between FED and the categorical diagnosis of PD was found in all the studies examined, regardless of the current or previous psychiatric disorders present in the subjects examined. This criterion, discriminating in other areas of investigation, will be examined later. However, in this outcome measure, the available data do not allow to draw meaningful conclusions on the comorbidity between FED and PD. A second result worthy of evidence but which still needs further investigation concerns the transversality of BPD in all three FEDs considered in this review, if not the three main FEDs according to the APA task force. In fact, it is interesting to note how, in the two studies that examined in greater depth the comorbidity between FED and personality clusters (Udo & Grilo, 2019; Valente et al., 2017), a statistically significant association emerges between BPD and FED, in particular with AN and BN. This result, in agreement with other findings in the literature (Martinussen et al., 2016; McDonald, 2019; Shah & Zanarini, 2018; Newton, 2019; Khosravi, 2020), could be due to the multiple facets of BPD and its traits, which covers various clinical areas (APA, 2014; Gestri, Pazzagli, & Ugolini, 2016). According to what was reported in a recent article by Newton (2019) (Newton, 2019) in fact, a comorbidity between BPD and FED emerges, in particular with: 20% of outpatient patients with bingeing / elimination conducts type AN and 50% of patients with BN (Newton, 2019; Maranon, Echeburia, & Grijalvo, 2007). Some transdiagnostic elements can therefore be identified through the two syndromes such as shared etiological factors as well as shared syndromic components such as: affective problems, interpersonal problems, problems with the self-concept, shared effects of trauma and impulsivity (Newton, 2019). Considering these multiple shared transdiagnostic elements, there is considerable evidence that transdiagnostic therapeutic approaches such as CBT-E lead to improvements in both syndromes. In conclusion, therefore, the co-occurrence between FED and BPD should be a strong predictor for severity, difficulty in commitment and adherence to treatment, as well as a risk factor for self-harm and suicidal behaviour (Newton, 2019). In support of these results, another recent study by Khosravi and colleagues (2020) states that there is a 65.4% prevalence of FED in patients with BPD (Khosravi, 2020), resulting in a partially overlapping total comorbidity rate. The third and fourth results, coming from the articles by Quirk and colleagues (2017) and Karjalainen and colleagues (2016) (Quirk et al., 2017; Karjalainen, Gillberg, Wentz, & Råstam, 2016), can be considered as a point of departure to carry out future studies to arrive at the formation of a common ground about the definition of FED as “complex cases” rather than as “disorders in comorbidity with”, as stated in the article by Dalle Grave and colleagues (2019) (Dalle Grave, Calugi, & Sartirana, 2019). In fact, from the analysis of the results of the two studies, emerge apparently opposite results but both lead to the falsification of the use of the term comorbidity: on the one hand, in fact they conclude by arguing that the presence of a PD during the life leads to a higher rate of comorbidity with FED than in subjects without PD; on the other hand (Karjalainen, Gillberg, Wentz, & Råstam, 2016) instead report that individuals with a FED do not have a greater psychiatric comorbidity than subjects without a FED. In light of these results then, why not consider FED as “complex cases”, as their (pathological) nature suggests? In fact, according to what is reported in the literature, it is difficult to assess the personality of patients with a FED as it is influenced by the specific psychopathology and its consequences (Dalle Grave, Calugi, & Sartirana, 2019; Garner & Dalle Grave, 1999). A fifth and final result that is particularly relevant, noteworthy and worthy of in-depth studies, comes from the article by Karjalainen and colleagues (2016). The subjects considered in this study, unlike the others, had a pre-existing psychiatric pathology – ESSENCE. It is interesting to note that the symptoms deriving from a FED in adult subjects with neuropsychiatric disorders tend to be over-represented and altered compared to the general population (7.9% vs 3% of the general population): this could be indicative of a vulnerability of subjects with ESSENCE to other psychiatric pathologies (Karjalainen, Gillberg, Wentz, & Råstam, 2016). Furthermore, the following study reveals a difference in eating pathology compared to subjects with ADHD and ASD (Boltri & Sapuppo, 2021). Adults with ASD appear to be less likely to try new, rich foods: this may reflect the stiffness component present within the ASD (Karjalainen, Gillberg, Wentz, & Råstam, 2016; Poljac, Hoofs, Princen, & Poljac, 2017), while individuals with ADHD show a greater tendency to think about calories, exercise and body fat distribution. Despite these results, however, the overlap between ESSENCE and FED is still insufficiently analysed in young adult / adult subjects (Karjalainen, Gillberg, Wentz, & Råstam, 2016), making generalization of the results highly problematic.
Summary of Limitations
The following systematic review offer us a very limited studies of comorbidity between FEDs and PDs; this can be seen as both a limitation and an interesting finding. To date, in fact, starting from the year of publication of the last review on the subject (Martinussen et al., 2016), there are a total of N = 4 articles (Karjalainen, Gillberg, Wentz, & Råstam, 2016; Quirk et al., 2017; Udo & Grilo, 2019; Valente et al., 2017) which treat the comorbidity between the two disorders. Furthermore, it is important to point out that in these four studies reported in the following review, not all of them treat the comorbidity between FED and PD as their primary research goal. This further complicates the situation, leading to a greater scarcity of accurate and comprehensive data on the subject in question. This limit is linked to one of the objectives that we have tried to pursue with this revision work: to update the state of the art, trying to bring to light in a critical way the large gap in the literature on pathologies that are currently very frequent, especially among young and causing considerable distress, further aggravated by the lack of information needed to deal with it. Secondly, it is possible to identify that, although the articles used were conducted and published posthumously to the publication of the DSM-5, different diagnostic reference criteria were used. For example, two of the four reported articles (Quirk et al., 2017; Valente et al., 2017) refer to the DSM-IV and DSM-IV-TR; while the other two remaining articles at DSM-5 (Udo & Grilo, 2019; Karjalainen, Gillberg, Wentz, & Råstam, 2016). This may have caused overestimation / underestimation of diagnoses given the changes in diagnostic criteria that were implemented in the transition from DSM-IV to DSM-5. Subsequently, as identified by Dalle Grave and colleagues (2019), there are a series of general limitations caused by the methodological problems of comorbidity studies that reflect the large variability of the results (Dalle Grave, Calugi, & Sartirana, 2019). Among these we find:
- Limited use of control groups: in the studies there is an infrequent, if not absent, use of control groups matched by sex and age.
- Inhomogeneous general clinical sample: samples with the same clinical characteristics were not examined in all studies. In fact, in one study (Karjalainen, Gillberg, Wentz, & Råstam, 2016) the sample consisted of a subject with pre-existing psychiatric pathologies of a different nature from those analysed in this review.
- Structuring of the samples: in the reported studies, the analysed samples included subjects with different proportions of diagnostic categories (FED and PD)
- Samples with limited numbers: large samples were not taken into consideration in all studies. In fact, in one study in particular (Karjalainen, Gillberg, Wentz, & Råstam, 2016), the small sample does not allow to draw statistically reliable conclusions.
- Use of different assessment tools: In the studies, different tools were used to assess the same disorders. For example: AUDADIS-5; EAT-26; SCID-I; SCID-I / NP for FED. SCID-II, SCID-5-PD, AUDADIS-5 for PDs.
- Chronological onset and causality: in the studies a distinction was not made – because it was risky – as to whether the comorbid disorder had occurred before or after the other disorder in question and vice versa. It was therefore not analysed whether the comorbid characteristics were secondary to FED or PD, in short, causality. This, in addition to being an intrinsic feature of cross-sectional studies, is also a delicate, risky and difficult question to address, as the personality of patients with a FED is influenced by specific psychopathology and therefore also by the consequences of malnutrition in some cases (Dalle Grave, Calugi, & Sartirana, 2019; Garner & Dalle Grave, 1999).
- Missing data regarding the number of patients belonging to a specific diagnosis (Valente et al., 2017)
Finally, not least, it can be noted that unlike a meta-analysis such as that of Martinussen and colleagues (Martinussen et al., 2016), a narrative review fails to provide a substantial quantitative summary of the literature.
Conclusions and Areas for Future Research
The studies reported and analysed summarize what is present in the literature about the comorbidity between FED and the categorical diagnosis of PD starting from 2014 until today. They would partially reflect the results obtained previously and summarized fully in the meta-analysis by Martinussen and colleagues (Martinussen et al., 2016).
The results of this systematic review in fact highlight a close co-occurrence between the two psychopathologies, as both include common transdiagnostic elements, but also a change in comorbidity between the two disorders. The main results obtained from the analysis of the identified articles, as also present in Table II above, are schematically listed below.
- AN ↔ BPD (cluster B) (p = 0.001); OCPD (cluster C) (p <0.05) (Udo & Grilo, 2019; Valente et al., 2017)
- BN ↔ BPD (cluster B) (p <.05); [STPD (cluster A) (p = 0.094) – tending to significance] (Valente et al., 2017)
- BED ↔ PPD (p = 0.034) and STPD (p <.01) (cluster A); APD (p <.01) and BPD (p <.01) (cluster B) (Valente et al., 2017; Udo & Grilo, 2019)
Furthermore, as recently confirmed by other authors (Bertelli et al., 2019), there are comorbid differences based on gender within cluster B (Valente et al., 2017):
- F = BPD and OCPD ↔ AN
- M = PPD ↔ BED
It therefore appears that, in females affected by AN, the prevailing PDs are BPD and OCPD; while in males with BED the prevalent PD is the PPD.
In light of these results, it is possible to make a comparison with the previous ones reported in the meta-analysis by Martinussen and colleagues (2014). A first comparison confirms what is reported in this review, namely: there is a close co-occurrence between any PD and FED (p <.001) (Martinussen et al., 2016). In particular, as mentioned in the limits section, it is possible to note that in the reference meta-analysis it is possible to have a greater quantity and quality of quantitative data available. Therefore, in addition to confirming the aforementioned comorbidities concerning the psychopathologies of AN and BN, Martinussen and colleagues add further specifications. For example, they report that AN and BN are both closely co-morbid not only with BPD (p <.001), but also with APD with p <.01 (Martinussen et al., 2016). Subsequently they report another data that is not reported in this review: the comorbidity between AN and BN and DPD (p <.001), as previously reported by other authors (Macías, Unikel, Cruz, & Caballero, 2003). This result may be inconsistent with the more recent ones as the meta-analysis by Martinussen and colleagues was not based on the DSM-5 criteria like some articles reported in this review.
It should be noted that this work adds, with respect to the reference meta-analysis, the data relating to the BED, although this disorder was already present within the DSM-IV they used. For this reason, it is not possible to make comparisons with previous literature, as it is also a relatively recent disorder. Currently, it is only possible to state that BED appears to be a disorder with PD of both clusters A and B; in particular, with the PPD and STPD, APD and BPD. However, it is important to increase research also for this neo-psychopathology, as the data available to us in the scientific literature are scarce and cannot be generalized.
Concluding and taking into account the results, limitations and purpose of this review, it would be interesting to investigate various aspects with future studies with the main purpose of filling the large gap in the scientific literature on the topic under consideration. This objective could be pursued by analysing various aspects, including:
- the transversality of BPD in the three main FEDs or vice versa. From the results of the following systematic review, it emerges that BPD is transdiagnostic to all three FEDs. An important aspect, worthy of further study, therefore, concerns the search for those particular aspects of BPD that are found in a transdiagnostic way in the three main FEDs and why. This is the rationale that could push today’s researchers to deepen the subject in a more exhaustive and precise way. In fact, currently, in the literature, there is little and varied information available to us on this topic. FEDs appear to be common among BPD patients, as documented by several cross-sectional studies (Zanarini, Gunderson, & Frankenburg, 1989; Zimmerman & Mattia, 1999; McGlashan, Grilo, & Skodol, 2000; Pope, Jonas, & Hudson, 1983; Coid, 1993), but without a precise specification of the common aspects. These studies report a prevalence of any FED in BPDs ranging between 14% and 53% (Shah & Zanarini, 2018). Instead, according to a more recent article by Newton (2019) it is possible to identify transdiagnostic elements between the two syndromes including etiological factors as well as shared syndromic components such as: negative self-evaluation, negative affect, affective and impulse dysregulation, interpersonal sensitivity (Newton, 2019). Two years earlier, an article by Sloan and colleagues (2017) pointed out that deficits in the regulation of emotions are implicated among various psychological disorders, highlighting this construct as the trans-diagnostic element between various disorders such as FED and BPD (Sloan et al., 2017). Despite these results, however, the need for further study is underlined.
- The influence of pre-existing psychiatric disorders on the diagnosis of FED or vice versa. From the results that emerged from the article by Karjalainen and colleagues (2015), a result emerges that could be highly influenced by some personological traits present in a transdiagnostic manner both in psychiatric disorders such as ADHD and ASD and in certain types of FEDs such as in AN. Among these, for example, as cited by the same authors, it is possible to identify that among individuals with ADHD thoughts regarding calories and exercise are more frequent, while subjects with ASD show symptoms related to stiffness (Karjalainen, Gillberg, Wentz, & Råstam, 2016). These are characteristics that can be found as risk factors even in subjects with a FED, as reported by a recent narrative review (Tistarelli, Fagnani, Troianiello, Stazi, & Adriani, 2020). However, the data available to us are insufficient. It is therefore important to deepen the subject, in particular to understand how some psychiatric disorders pre-existing to FED (ADHD, ASD) can affect the diagnosis of FED and how much vice versa.
- The multifactorial etiology of FED is now known in the literature: this means that both the origin and development of the disorder are determined by a multiplicity of variables, including psychological, evolutionary and biological factors. The disease does not therefore appear to be triggered or influenced by a single variable, but by multiple ones (Marucci & Dalla Ragione, 2007; Cotugno & Sapuppo, 2019). Hence, therefore, the consideration that future research can critically investigate the effectiveness and development of forms of treatment that address this multifactorial nature.
Conflict of Interest Statement
All authors declare that they have no conflict of interests.
Authors Contributions
Both authors give substantial contributions to the conception or design of the work and to the interpretation of data. G.S. drafting the work and W.S. revising it critically and both give the approval of the version to be published.
References
American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders: DSM-5 (5th ed.). Washington DC: American Psychiatric Association.
American Psychiatric Association (2014). Manuale Diagnostico e Statistico dei Disturbi Mentali (quinta edizione): DSM-5. (M. Biondi, A cura di) Milano: Raffaello Cortina Editore.
Bertelli, S., Boschetti, F., Chinello, A., Faggioli, S. C., Dolci, V., Faraci, G., . . . Zappa, L. E. (2019). Anoressia e gravidanza: Percorsi di cura, vissuti psicopatologici, ricerca clinica. (L. E. Zappa, A cura di) Milano: FrancoAngeli.
Boltri, M., & Sapuppo, W. (2021). Anorexia Nervosa and Autism Spectrum Disorder: A Systematic Review. Psychiatry Research, 306, 114271. https://doi.org/10.1016/j.psychres.2021.114271
Coid, J. W. (1993). An affective syndrome in psychopaths with borderline personality disorder? British Journal of Psychiatry, 641-650. https://doi.org/10.1192/bjp.162.5.641
Cotugno, A., Sapuppo, W. (2019). Il trattamento cognitivo-comportamentale: dalle caratteristiche cliniche all’intervento multiprofessionale integrato. In Spitoni G.F. & Aragona M. (ed.), Manuale dei disturbi alimentari (pp. 297 – 320). Roma: Carocci.
Dalle Grave, R., Calugi, S., & Sartirana, M. (2019). Comorbilità vera e comorbilità spuria nei disturbi dell’alimentazione. IJEDO, 1-7. https://doi.org/10.32044/ijedo.2019.01
Friborg, O., Martinussen, M., Schmierer, P., Overgard, K. T., Kaiser, S., & Rosenvinge, J. H. (2014). Personality disorders in eating disorder NOS and binge eating disorder (BED). A meta-analysis of comorbidity studies. Journal of Nervous and Mental Disease, 202, pp. 119-125. https://doi.org/10.1097/NMD.0000000000000080
Garner, D. M., & Dalle Grave, R. (1999). Terapia cognitivo comportamentale dei disturbi dell’alimentazione. Verona: Positive Press.
Gestri, C., Pazzagli, C., & Ugolini, E. (2016, Giugno). Il Disturbo Borderline di Personalità. Modelli e Strumenti per la diagnosi e il trattamento. I Quaderni della Fondazione degli Psicologi della Toscana, 2, p. 1-17.
Jahan, N., Naveed, S., Zeshan, M., & Tahir, M. (2016). How to Conduct a Systematic Review: A Narrative Literature Review. Cureus. https://doi.org/10.7759/cureus.864
Karjalainen, L., Gillberg, C., Wentz, E., & Råstam, M. (2016). Eating disorders and eating pathology in young adult and adult patients with ESSENCE. Comprehensive Psychiatry, 66, 79-86. https://doi.org/10.1016/j.comppsych.2015.12.009
Khosravi, M. (2020). Eating disorders among patients with borderline personality disorder: understanding the prevalence and psychopathology. Journal of Eating Disorder, 8(38), 1-9. https://doi.org/10.1186/s40337-020-00314-3
Macías, L. G., Unikel, C., Cruz, C., & Caballero, A. (2003, Giugno). Personalidad y trastornos de la conducta alimentaria. Salud Mental, 26(3), p. 1-8.
Maranon, I., Echeburia, E., & Grijalvo, J. (2007). Are there more personality disorders in treatment seeking patients with eating disorders than in other kinds of psychiatric patients? International Journal of Clinical and Health Psychology, 7, 283-293.
Martinussen, M., Friborg, O., Schmierer, P., Kaiser, S., Overgard, K. T., Neunhoeffer, A. L., . . . Rosenvinge, J. H. (2016, Settembre 12). The comorbility of personality disorders in eating disorders: a meta-analysis. International Journal of Eating and Weight Disorders. https://doi.org/10.1007/s40519-016-0345-x
Marucci, S., & Dalla Ragione, L. (2007). L’anima ha bisogno di un luogo. Disturbi alimentari e ricerca dell’identità. Milano: Tecniche nuove.
McDonald, S. (2019). Understanding the genetics and epigenetics of bulimia nervosa/bulimia spectrum disorder and comorbid borderline personality disorder (BN/BSD-BPD): a systematic review. Eating and Weigh Disorders – Studies on Anorexia, Bulimia and Obesity, 24, 799-814. https://doi.org/10.1007/s40519-019-00688-7
McGlashan, T. H., Grilo, C. M., & Skodol, A. E. (2000). The collaborative Longitudinal Personality Disorders Study: baseline Axis I/II and II/II diagnostic co-occurrence. Acta Psychiatrica Scandinavica, 256-264. https://doi.org/10.1034/j.1600-0447.2000.102004256.x
Mitchell, K. S., Wolf, E. J., Reardon, A. F., & Miller, M. W. (2014). Association of eating disorder symptoms with internalizing and externalizing dimensions of psychopathology among men and women. International Journal of Eating Disorders, 860-869. https://doi.org/10.1002/eat.22300
Moher, D., Liberati, A., Shamseer, L., Clarke, M., Ghersi, D., Patticrew, M., . . . Group, T. (2015, Luglio). Linee guida per il reporting di revisioni sistematiche e meta-analisi : il PRISMA Statement. Evidence, 7(6).
Newton, R. (2019, Giugno 3). Borderline personality disorder and eating disorders: a trans-diagnostic approach to unravelling diagnostic complexity. Australasian Psychiatry, 1-3. https://doi.org/10.1177/1039856219852297
Page, M.J., McKenzie, J.E., Bossuyt, P.M., Boutron, I., Hoffmann, T.C., Mulrow, C.D., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. https://doi.org/10.1136/bmj.n71
Poljac, E., Hoofs, V., Princen, M. M., & Poljac, E. (2017). Understanding Behavioural Rigidity in Autism Spectrum Conditions: The Role of Intentional Control. Journal of Autism and Developmental Disorders, 47, 714-727. https://doi.org/10.1007/s10803-016-3010-3
Popay, J., Roberts, H., Sowden, A., Petticrew, M., Arai, L., Rodgers, M., . . . Duffy, S. (2006). Narrative Synthesis in Systematic Reviews: A Product from the ESRC Methods Programme. ESRC Methods Programme. https://doi.org/10.13140/2.1.1018.4643
Pope, H. G., Jonas, J. M., & Hudson, J. I. (1983). The validity of DSM-III Borderline Personality Disorders. A phenomenologic, family history, treatment response, and long-term follow-up study. Archives Of General Psychiatry, 23-30. https://doi.org/10.1001/archpsyc.1983.01790010025003
Quirk, S., Berk, M., Pasco, J. A., Brennan-Olsen, S. L., Chanen, A. M., Koivumaa-Honkanen, H., . . . Williams, L. J. (2017). The prevalence, age distribution and comorbidity of personality disorders in Australian women. Australian and New Zealand Journal of Psychiatry, 51(2), 141-150. https://doi.org/10.1177/0004867416649032
Rosenvinge, J. H., Martinussen, M., & Ostensen, E. (2000). The comorbidity of Eating Disorders and personality disorders: a meta-analytic review of studies published between 1983 and 1998. Eating and Weight Disorders, 5, pp. 52-61. https://doi.org/10.1007/BF03327480
Rosenvinge, J. H., & Pettersen, G. (2015). Epidemiology of eating disorders part III: social epidemiology and case definitions revisited. Advances in Eating Disorders: Theory, Research and Practice, 320-336. https://doi.org/10.1080/21662630.2015.1022197
Sapuppo, W., Ruggiero, G. M., Caselli, G., Sassaroli S. (2018). The body of cognitive and metacognitive variables of eating disorders: need of control, negative beliefs about worry uncontrollability and danger, perfectionism, self-esteem, and worry. Israel Journal of Psychiatry and related Sciences, 55,1. PMID: 29916407. https://pubmed.ncbi.nlm.nih.gov/29916407/
Shah, R., & Zanarini, M. (2018, Dicembre). Comorbidity of Borderline Personality Disorder: Current Status and Future Directions. Psychiatric Clinics of North America, 41(4), 583-593. https://doi.org/10.1016/j.psc.2018.07.009
Sloan, E., Hall, K., Moulding, R., Bryce, S., Mildred, H., & Staiger, P. (2017). Emotion regulation as a transdiagnostic treatment construct across anxiety, depression, substance, eating and borderline personality disorders: A systematic review. Clinical Psychological Review, 141-163. https://doi.org/10.1016/j.cpr.2017.09.002
Tistarelli, N., Fagnani, C., Troianiello, M., Stazi, M. A., & Adriani, W. (2020). The nature and nurture of ADHD and its comorbidities: A narrative review on twin studies. Neuroscience and biobehavioral reviews, 109, 63-77. https://doi.org/10.1016/j.neubiorev.2019.12.017
Udo, T., & Grilo, C. M. (2019). Psychiatric and medical correlates of DSM-5 eating disorders in a nationally representative sample of adults in the United States. International Journal of Eating Disorders, 52(1), 42-50. https://doi.org/10.1002/eat.23004
Valente, S., Di Girolamo, G., Forlani, M., Biondini, A., Scudellari, P., De Ronchi, D., & Atti, A. R. (2017). Sex-specific issues in eating disorders: a clinical and psychopathological investigation. Eating and Weight Disorders, 22(4), 707-715. https://doi.org/10.1007/s40519-017-0432-7
Zanarini, M. C., Gunderson, J. G., & Frankenburg, F. R. (1989). Axis I phenomenology of borderline personality disorder. Comprehensive Psychiatry, 30(2), 149-156. https://doi.org/10.1016/0010-440X(89)90067-9
Zimmerman, M., & Mattia, J. I. (1999). Axis I diagnostic comorbidity and borderline personality disorder. Comprehensive Psychiatry, 40(4), 245-252. https://doi.org/10.1016/s0010-440x(99)90123-2