Number and characteristics of patients seeking treatment for eating disorders at a CBT-E clinical service before and during the COVID-19 pandemic
Riccardo Dalle Grave1,2, Elisa Chignola2, Cecilia Franchini2, Laura Macrì2, Anna Chiara Manganotti2, Valeria Monti2, Nicole Morandini2, Massimiliano Sartirana2, Simona Calugi1
1 Department of Eating and Weight Disorders, Villa Garda Hospital, Garda (VR), Italy
2 Associazione Disturbi Alimentari (ADA), Verona, Italy
Abstract
This retrospective study aimed to assess the number, demographic and clinical characteristics of patients seeking treatment for eating disorders at a clinical service specialized in delivering enhanced cognitive behavior (CBT-E) before (01/01/2018 – 08/03/2020) and during (09/03/2020 – 31/12/2021) the coronavirus (COVID-19) pandemic. A larger number of adults than adolescents sought treatment both before (121 [66%] vs. 62 [44%]) and during the COVID-19 pandemic (108 [53%] vs. 95 [47%]) (chi-squared=6.66, p=0.010). However, the percentage of adolescents seeking treatment was higher in the pandemic than in pre-pandemic years (60.5% vs. 39.5%). On the contrary, the rate of adults with an age of ≥25 years was lower during the COVID-19 pandemic (chi-square=8.71, p=0.033). No significant difference was found in demographics, clinical characteristics, and DSM-5 diagnoses between patients seeking treatment before and during the COVID-19 pandemic. In conclusion, the results show a significant increase in adolescent patients seeking outpatient CBT-E during the COVID-19 pandemic.
Keywords
COVID-19
Coronavirus disease
Eating disorders
Adolescents
Adults
Cognitive behavior therapy
Public health
Introduction
The coronavirus disease (COVID-19) pandemic and the social and physical distancing measures introduced by governments to counter its spread have been associated with an increased incidence of eating disorders (Taquet, Geddes, Luciano, & Harrison, 2021). Some authors and studies also reported worsening of eating-disorder and general psychopathology in people with eating disorders (Dalle Grave 2020; Devoe et al., 2022; Monteleone, 2021). These dramatic changes have produced a noticeable increase in acute and routine referrals (Richardson, Phillips, & Paslakis, 2021; Rodgers et al., 2020) and inpatient admissions for eating disorders, particularly in adolescents (Haripersad et al., 2021; Lin et al., 2021; Marino et al., 2021; Solmi, Downs, & Nicholls, 2021).
The present study aimed to assess the number, demographic and clinical features of patients seeking treatment at an enhanced cognitive behavior (CBT-E) outpatient clinical service for eating disorders before and during the COVID-19 pandemic.
Methods
Study design and participants
This retrospective study was conducted on a sample of consecutively seeking treatment patients with eating disorders at the Associazione Disturbi Alimentari (ADA) before (01/01/2018 -08/03/ 2020) and during (09/03/2020 – 31/12/2021) the COVID-19 pandemic. ADA is a secondary care clinical service specialized in delivering the adolescent (Dalle Grave & Calugi, 2020) and adult version (Fairburn et al., 2008) of CBT-E.
Participants were referred by primary care physicians, pediatricians, or other health stakeholders. All meet the Diagnostic and Statistical Manual of Mental Disorders, edition 5 (DSM-5) (American Psychiatric Association, 2013), diagnostic criteria for a feeding and eating disorder assessed by an eating disorder specialist.
Informed written consent for the collection and anonymous processing of their clinical data were provided by participants (and the parent(s) and/or legal guardian(s) of those under 18 years of age). As all treatment and assessment procedures were performed as part of routine clinical practice rather than purely for research, no ethical clearance was sought for the study following Italian National Health System ethics guidelines.
Measurement
- Body weight and body mass index (BMI). The BMI was calculated by dividing the body weight, measured on a beam-balance scale, by the square of the height, measured on a wall-mounted stadiometer.
- Age at onset of the eating disorder.
- Duration of illness.
- Minimum and maximum body weight.
- DSM-5 diagnosis. The DSM-5 diagnosis was assessed by expert clinicians.
Statistical analyses
All data are presented as mean and standard deviation or number and percentage, as appropriate. Chi-square test and t-test for independent variables were used to compare clinical and demographic variables before and during the COVID-19 pandemic.
Results
Three hundred eighty-six patients with eating disorders sought treatment at the CBT-E clinical service in the COVID-19 pre-pandemic and pandemic years (157 [40.7%] adolescents and 229 [59.3%] adults).
Overall, a significantly larger proportion of adult than adolescents contacted the clinical service both before and during the COVID-19 pandemic years (chi-squared=6.66, p=0.010). However, before and during the COVID-19 pandemic, the number of seeking-treatment adolescent patients increased from 62 (39.5%) to 95 (60.5%), while the number of adult patients decreased from 121 (52.8%) to 108 (47.2%).
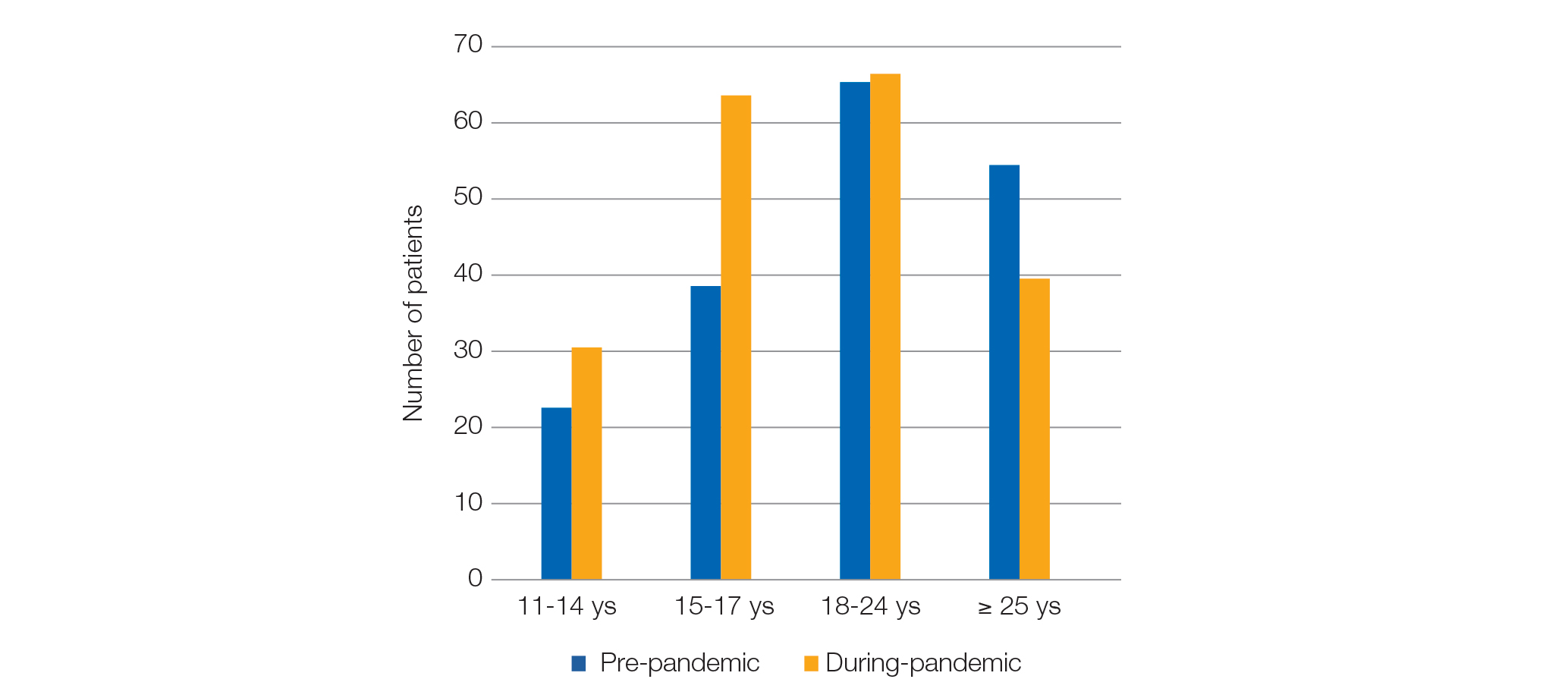
Figure 1 shows the age distribution of patients who contacted the CBT-E clinical service before and during the COVID-19 pandemic. A significantly larger percentage of adolescents sought treatment during the pandemic than before the COVID-19 pandemic. On the contrary, a significantly smaller percentage of adults ≥ 25 years contacted the same CBT-E clinical service during the COVID-19 pandemic (chi-square=8.71, p=0.033).
Figure 1. Age distribution of patients contacting the CBT-E clinical service before and during COVID-19 years
The demographic and clinical characteristics of the adolescent and adult patients seeking treatment at the CBT-E clinical service before and during COVID-19 are similar, as shown in Table 1.
The eating disorder DSM-5 diagnosis of adolescent and adult patients contacting the CBT-E clinical service in the COVID-19 pre- and during pandemic years are shown in Table 2.
Table 1. Demographic and clinical characteristics of the adolescents and adult patients seeking treatment at a CBT-E clinical service before and during the COVID-19 pandemic years
| Adolescents (n=157) | Adults (n=229) | |||
|---|---|---|---|---|
| Before pandemic (n=62) | During pandemic (n=95) | Before pandemic (n=121) | During pandemic (n=108) | |
| Gender, N (%) female | 58 (93.4%) | 92 (96.8%) | 114 (94.2%) | 100 (92.6%) |
| Age, years, mean (SD) | 14.9 (1.6) | 15.2 (1.5) | 26.8 (9.1) | 25.9 (9.6) |
| Age at onset, years, mean (SD) | 14.0 (1.6) | 14.3 (1.4) | 19.1 (6.3) | 19.2 (6.0) |
| Duration of illness, years, mean (SD) | 1.0 (1.2) | 0.9 (1.1) | 7.1 (8.2) | 6.2 (7.6) |
| Body mass index, mean (SD) | 18.6 (3.9) | 17.8 (2.9) | 19.9 (4.8) | 19.4 (5.4) |
| Minimum weight, kg, mean (SD) | 45.3 (10.6) | 46.1 (9.2) | 54.8 (90.2) | 45.3 (0.3) |
| Maximum weight, kg, mean (SD) | 56.8 (13.1) | 56.9 (8.8) | 64.4 (12.8) | 64.7 (13.6) |
No significant differences were found.
Table 2. The distribution of eating-disorder diagnoses (DSM-5) among consecutive adolescent (11-17 years) and adult patients (≥ 18 years) seeking treatment at a CBT-E clinical before and during the COVID-19 pandemic years
| Adolescents (n=157) | Adults (n=229) | |||
|---|---|---|---|---|
| Diagnosis | Before pandemic (n=62) | During pandemic (n=95) | Before pandemic (n=121) |
During pandemic (n=108) |
| Anorexia nervosa | 36 (58.1%) | 66 (69.5%) | 52 (43.0%) | 53 (49.1%) |
| Bulimia nervosa | 7 (11.3%) | 7 (7.4%) | 25 (20.7%) | 19 (17.6%) |
| Binge-eating disorder | 4 (6.5%) | 4 (4.2%) | 17 (14.0%) | 16 (14.8%) |
| Other specified eating disorders | ||||
| Atypical anorexia nervosa | 4 (6.4%) | 13 (13.8%) | 9 (7.5%) | 7 (6.5%) |
| Bulimia nervosa (of low frequency and/or limited duration) | 0 | 1 (1.1%) | 2 (1.7%) | 0 |
| Binge-eating disorder (of low frequency and/or limited duration) | 1 (1.6%) | 0 | 1 (0.8%) | 1 (0.9%) |
| Purging disorder | 0 | 1 (1.1%) | 2 (1.7%) | 3 (2.8%) |
| Night eating syndrome | 0 | 0 | 1 (0.8%) | 1 (0.9%) |
| Other non-specified eating disorders | 7 (11.3%) | 3 (3.2%) | 6 (5.0%) | 0 |
No significant differences were found.
Discussion
This study aimed to assess the number, the demographic and clinical characteristics of seeking treatment patients with eating disorders at an Italian CBT-E clinical service before and during the COVID-19 pandemic.
We found two main findings. The first is that a larger number of adults than adolescents contacted the CBT-E clinical service both before and during the pandemic. However, considering the age distribution of patients, a larger proportion of adolescents, mainly between 15 and 17 years, contacted the CBT-E clinical service in the pandemic than in the pre-pandemic period. On the contrary, a smaller proportion of adults aged ≥25 years sought treatment during the pandemic. This finding confirm previous data reporting a greater demand for help, especially from adolescents with eating disorders, during the COVID-19 pandemic (Richardson et al., 2021; Rodgers et al., 2020).
The second finding concerns adult and adolescent patients’ demographic and clinical characteristics. Contrary to previous studies, we did not find a significant difference in the two groups on gender, age, age at onset, duration of illness, BMI, and minimum and maximum weight before and during the COVID-19 pandemic years. Similarly, no difference was found when considering the DSM-5 diagnosis, although the lack of specific data about eating-disorder psychopathology limits this conclusion. However, the study’s strength is that the data were collected in a specialized CBT-E clinical service operating in a real-world setting.
In conclusion, this retrospective study found a significant increase in adolescent patients seeking outpatient CBT-E during the COVID-19 pandemic and indicates the need to allocate more financial and clinical resources to treat young with eating disorders with this evidence-based treatment.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders, (DSM-5). Arlington: American Psychiatric Publishing.
Dalle Grave , R. (2020, 21 March 2020). Coronavirus Disease 2019 and Eating Disorders. Retrieved from https://www.psychologytoday.com/intl/blog/eating-disorders-the-facts/202003/coronavirus-disease-2019-and-eating-disorders
Dalle Grave, R., & Calugi, S. (2020). Cognitive behavior therapy for adolescents with eating disorders. New York: Guilford Press.
Devoe, D. J., Han, A., Anderson, A., Katzman, D. K., Patten, S. B., Soumbasis, A., . . . Dimitropoulos, G. (2022). The impact of the COVID-19 pandemic on eating disorders: A systematic review. International Journal of Eating Disorders. doi:10.1002/eat.23704
Fairburn, C. G., Cooper, Z., Shafran, R., Bohn, K., Hawker, D., Murphy, R., & Straebler, S. (2008). Enhenced cognitive behavior therapy for eating disorders: The core protocol. In C. G. Fairburn (Ed.), Cognitive behavior therapy and eating disorders (pp. 45-193). New York: Guilford Press.
Haripersad, Y. V., Kannegiesser-Bailey, M., Morton, K., Skeldon, S., Shipton, N., Edwards, K., . . . Martin, A. C. (2021). Outbreak of anorexia nervosa admissions during the COVID-19 pandemic. Archives of Disease in Childhood, 106(3), e15. doi:10.1136/archdischild-2020-319868
Lin, J. A., Hartman-Munick, S. M., Kells, M. R., Milliren, C. E., Slater, W. A., Woods, E. R., . . . Richmond, T. K. (2021). The Impact of the COVID-19 Pandemic on the Number of Adolescents/Young Adults Seeking Eating Disorder-Related Care. Journal of Adolescent Health, 69(4), 660-663. doi:10.1016/j.jadohealth.2021.05.019
Marino, A., Gliubizzi, C., Reina, F., Nocera, G. M., Marchese, F., & Trapolino, E. (2021). Increase in admissions for anorexia nervosa after lockdown measures: Focus on a children’s neuropsychiatry unit. General Hospital Psychiatry, 72, 147-148. doi:10.1016/j.genhosppsych.2021.06.005
Monteleone, P. (2021). Eating Disorders in the Era of the COVID-19 Pandemic: What Have We Learned? International Journal of Environmental Research and Public Health, 18(23). doi:10.3390/ijerph182312381
Richardson, C., Phillips, S., & Paslakis, G. (2021). One year in: The impact of the COVID-19 pandemic on help-seeking behaviors among youth experiencing eating disorders and their caregivers. Psychiatry Research, 306, 114263. doi:10.1016/j.psychres.2021.114263
Rodgers, R. F., Lombardo, C., Cerolini, S., Franko, D. L., Omori, M., Fuller-Tyszkiewicz, M., . . . Guillaume, S. (2020). The impact of the COVID-19 pandemic on eating disorder risk and symptoms. International Journal of Eating Disorders, 53(7), 1166-1170. doi:10.1002/eat.23318
Solmi, F., Downs, J. L., & Nicholls, D. E. (2021). COVID-19 and eating disorders in young people. Lancet Child Adolesc Health, 5(5), 316-318. doi:10.1016/s2352-4642(21)00094-8
Taquet, M., Geddes, J. R., Luciano, S., & Harrison, P. J. (2021). Incidence and outcomes of eating disorders during the COVID-19 pandemic. The British Journal of Psychiatry, 1-3. doi:10.1192/bjp.2021.105